Updated: August 2023

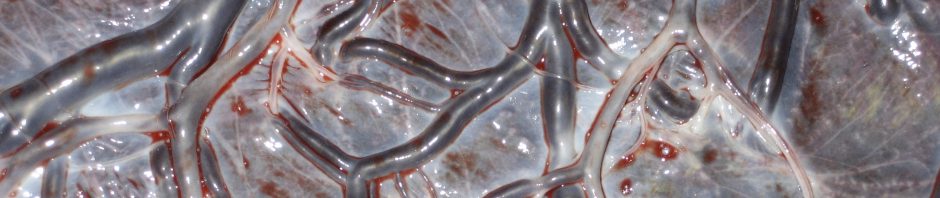
Most women will sustain some damage to their perineum during birth (AIHW 2023). Around half will have a tear or graze in the skin and/or vaginal wall (1st / 2nd degree). A quarter will be cut with episiotomy scissors. Occasionally (2% of non-instrumental vaginal births / 5.7% of instrumental births) significant tearing occurs that extends into the anal sphincter (3rd / 4th degree). This post will discuss ‘protecting the perineum’ and was initially based on a literature review. You can find the full literature review and reference list in my thesis. I have updated the post regularly since then and have added new references in the text.
Care providers often consider themselves to be ‘perineal protectors’ tasked with preventing women from tearing. There is currently a lot of effort and money being put into trying to reduce significant tearing (see this post). And of course the approach taken to ‘protect the perineum’ reflects the birth culture in general ie. that women’s bodies are dangerous, and risk management involves carrying out interventions to minimise that risk. I think the truth is the other way around. What we do is usually the risk, and risk management should be about supporting physiology and instinct. Only intervening when there is a deviation from physiology.
Before we look at what the research says, bear in mind that research about birth outcomes is carried out on general populations i.e primarily on women having medically managed births. These types of births often involve interventions that increase tearing eg. syntocinon, directed pushing, instrumental birth etc. We don’t have any good research about what protects the perineum during an uninterrupted, physiological birth where tearing rates are much lower.
Before birth
Fixed factors
Some factors that increase the chance of tearing are impossible or very difficult to control (Dahlen et al. 2015):
- a big baby
- first vaginal birth
- high weight gain in pregnancy
- higher socioeconomic circumstances
- older and younger maternal age
- ethnicity (Caucasian and Asian)
- short perineal body
- nutritional status
- abnormal collagen synthesis
Preparing the perineum for birth
Suggesting there is a need to ‘prepare’ for birth contradicts the fact that women’s bodies are perfectly capable of preparing for birth without intervention. However, perineal stretching massage can increase some women’s confidence in their body’s ability to stretch and open for their baby. On the other hand, plenty of women don’t prepare in this way, and whether you have confidence in your body or not, your perineum will stretch.
A number of guidelines recommend that women should be encouraged to massage their perineums during pregnancy to reduce the chance of tearing. The reference cited to support this recommendation is a Cochrane Review. However, the review did not conclude that massage reduced the chance of tearing. It found that women having their first baby who did perineal massage were less likely to have an episiotomy – not a tear. An episiotomy is an external factor and is dependent on the individual care provider rather than the woman’s anatomy. Perhaps perineal massage helps women to fit unnecessary birthing timeframes prescribed by hospitals, therefore avoid being cut?
There are also perineal stretching devices being marketed to women. The websites for these products make bold unsubstantiated statements. One brand simply states figures with no citation. Another popular brand has a webpage listing ‘studies’. However, these studies are pilot studies, study protocols or are very poor quality and old. Interesting, the only good quality research I can find into this device is not included on the brand website. This large RCT found that the stretching device did not reduce the chance of any type of perineal tearing, episiotomy, levator ani damage or anal sphincter trauma. Instead, it increased the rate of external anal sphincter damage. The researchers conclude that “antenatal use of the Epi-No device is unlikely to be clinically beneficial in the prevention of intrapartum levator ani damage, or anal sphincter and perineal trauma.” Personally I worry about potential long term effects of repeatedly stretching the perineum to the size of a baby’s head. Although a woman may give birth a number of times during her life, she will usually have more than a day between each baby’s head stretching her vagina. I’d be interested to see some long term studies into pelvic floor outcomes after the use of these devices.
During birth
Birth is where all of the care provider activity focuses. It was seeing all of the fussing and fiddling carried out as babies were born that sent me in the direction of a PhD. I could not understand why such a physiological and instinctive bodily process required so much directing and doing. I still don’t. I suggest that before (or after) you read this post, you read supporting women’s instinctive pushing behaviour during birth. Of course, most women do not have an undisturbed birth, therefore are not necessarily connected in with what is going on in their body. In these cases it may be appropriate to intervene (with consent).
General factors known to increase the chance of tearing during birth are (Dahlen et al. 2015):
- position of baby – larger diameter of head presenting
- midline episiotomy (see below)
- instrumental birth (particularly forceps)
- ‘prolonged second stage’ – likely because this results in an instrumental birth
- syntocinon (pitocin) use in women having their second or more vaginal birth
- shoulder dystocia
The main principles involved in reducing the chance of tearing is the capacity for stretch and ‘give’ in the perineal tissues.
The location of birth is also a factor with hospital birth increasing the chance of perineal tearing.
Positions
Some birth positions assist with the principle above ie. the maximise the capacity for stretch. The two positions that involve the least chance of tearing (side lying and hands/knees) do not involve stretched-wide legs and therefore stretched perineal tissue. In addition the pressure of the baby’s head is towards the front of the mother rather than directly onto the perineum. In contrast, positions that make the perineum tight and stretched, and place all of the pressure of the baby’s head directly onto the perineum increase the chance of tearing: semi-supine (sitting upright and reclined – the TV/film birth position); squatting; and lithotomy.
Many women will instinctively close their legs during crowning. I have seen midwives push women’s legs back open or say ‘keep your legs open’. Closing the legs, or bringing them in from a wide-open position protects the perineum. Try it yourself… open your legs wide and bring them up towards your chest – stranded beetle position – and feel what happens to your perineum. Now close your legs a little and bring them down away from your chest – feel how much more ‘give’ there is in your perineum when it is not stretched out. It can now respond to the stretch required by the baby’s head without already being stretched out sideways. As for whether closing your legs will stop a baby from coming out… it may slow it down, but that baby is coming out. I have seen a woman birth on her side with her legs crossed – her baby came out from behind.
Standing up-right can result in a quick birth – particularly for women who have previously given birth – increasing the chance of tearing. It is not a position many women stay in to birth unless they have been directed to get into it.
Guidelines and training are reinforcing the need for the care providers to ‘visualise the perineum’ during birth. I’m not sure how that is supposed to prevent tearing. However, it does increase the chance the care provider will intervene. This approach is leading to more women being directed into positions to facilitate this – unfortunately positions that increase the chance of tearing.
Directed pushing
Guidelines recommend that ‘good communication’ is required between the care provider and woman to ensure a slow birth and minimise tearing. However, this is unnecessary if the woman is birthing instinctively. The intense sensations experienced during crowning usually result in the woman ‘holding back’ while the uterus continues to push the baby out slowly and gently. Often women will hold their baby’s head and/or their vulva. I have witnessed one mother attempt to push her baby back in (you know who you are) – it was unsuccessful but gave us a giggle afterwards. Telling a woman to stop pushing, pant or ‘give little pushes’ distracts her at a crucial moment, and suggests that you are the expert in her birth, which you are not. She is the one with a baby’s head in her vagina – leave it to her. Of course, if you have been shouting at her to ‘Puuuush’ with every contraction before crowning – she will be listening to you, not her body…
Warm water
Some women find having a warm compress held against their perineum as the baby crowns helps to ease the sensations of stretching. Others, hate it and find it intrusive. A Cochrane review found that warm compresses did not increase the chance of having an intact perineum or decrease the chance for suturing. However, it did reduce the chance of a very severe tear (3rd or 4th degree).
Waterbirth is another way of bathing the perineal tissue in warm water – and unlike warm compresses, makes it difficult for anyone apart from the birthing woman to touch her perineum or baby during birth.
‘Hands on’ techniques
Hands on techniques aimed at slowing the birth of the baby and supporting the perineal tissues are routinely used by many care providers. However, a systematic literature review concluded that: “The hands-poised [off] technique appeared to cause less perineal trauma and reduced rates of episiotomy. The hands-on technique resulted in increased perineal pain after birth and higher rates of postpartum haemorrhage.” A Cochrane Review found that ‘hands on’ techniques did not reduce the chance of tearing and increased the chance of having an episiotomy. And a recent Australian study found that ‘hands on’ increased the chance of tearing for women having their second or more vaginal birth.
No research has explored women’s experiences of a ‘hands on’ approach. And, I am yet to hear a midwife or obstetrician ask for permission before placing their hands on the woman and baby.
Perineal massage
Massaging the perineum as the baby is trying to be born concerns me for a number of reasons. It makes me really uncomfortable to watch lots of ‘activity’ being done to a woman’s body while she is trying to birth. I have seen some very brutal versions of ‘perineal massage’ done to women; and I am guessing/hoping that most of the women in these studies had epidurals. However, the Cochrane Review above suggests that this type of massaging can reduce the chance of significant tears (3rd and 4th degree) not the usual (1st and 2nd degree). Significant tearing is rare (around 3%) – so the intervention needs to be weighed up with the risks of additional pain and disturbance to physiology. Also, in order to perform this intervention effectively the woman needs to be in a position that increases her chance of tearing ie. on her back / semi-reclined.
Episiotomy
An episiotomy involves a deep cut into the perineal muscles and skin ie. creating perineal trauma. Episiotomies used to be rare in midwifery practice. I have carried out three in my career, and with hindsight I think two were unnecessary. However, there is a resurgence thanks to a new wave of perineal focused intervention packages, and confusing research summaries and clinical guidelines.
For example, a Cochrane Review examining ‘selective’ vs ‘routine’ episiotomy concluded that: “In women where no instrumental delivery is intended, selective episiotomy policies result in fewer women with severe perineal/vaginal trauma.” This seems to have been interpreted as ‘selective episiotomy reduces severe tearing’ rather than ‘in comparison to routine episiotomy’. Interestingly, the review does not include information about what indications are included in a ‘selective’ approach, or the evidence supporting those indications.
There is some evidence about outcomes relating to the types of episiotomies used – mid-line (down toward the anus) vs medio-lateral (60 degree angle). A mid-line episiotomy contributes to the risk of severe perineal trauma by increasing the chance the cut will extend (Lappen & Gossett 2014). However, a medio-lateral episiotomy cuts through more nerves and perineal structures (Patel et al. 2018). We are only just beginning to understand the complex anatomy of the clitoris – a structure that is cut during a medio-lateral episiotomy. This type of episiotomy is associated “with a decreased sexual functioning as well as sexual desire, arousal and orgasm within postpartum five years” (Dogan et al. 2017).
Even if episiotomy does reduces the chance of severe tearing (which we don’t have the evidence for) – having an episiotomy during a non-instrumental vaginal birth would be trading a 2% chance of significant tearing with 100% chance of perineal damage via a cut.
After birth
Suturing
Tearing is a normal part of the birth process, and the body usually heals well. The vaginal wall is a mucous membrane and heals very fast (like the mouth). Suturing is the most common method of perineal repair. Whether to suture or not should be the woman’s decision. In relation to 2nd degree tears (the most common) the need to suture is debatable if the tear aligns well and is not bleeding. A Cochrane Review concluded:
“…at present there is insufficient evidence to suggest that one method is superior to the other with regard to healing and recovery in the early or late postnatal periods. Until further evidence becomes available, clinicians’ decisions whether to suture or not can be based on their clinical judgement and the woman’s preference after informing them about the lack of long-term outcomes and possible chance of slower wound healing process, but possible better overall feeling of well being if left un-sutured.”
In my own experience as a midwife found that un-sutured perineums heal very quickly and with far less pain than sutured perineums.
In summary
There is very little care providers can do to protect women’s perineums using interventions. Instead, we need to encourage women to trust that their body has an innate ability to birth their baby; that perineal tearing is a normal part of birth; and that the body will heal itself.
If you enjoyed this post, you can find more of my work in the following resources:
- Dr Rachel Reed YouTube Channel
- The Midwives’ Cauldron Podcast
- Books
- Courses
- Reclaiming Childbirth Collective
Join my Mailing List for a monthly newsletter and to stay up to date with new content.






Can’t begin to imagine how irritating, distracting having someone’s hands there would have been whilst trying to ease my baby out gently during this most challenging stage of my labour/ birth. The issue of consent you raise is so true, as a student I have never once heard a midwife or ob ask a women’s permission to be hands on during this stage.
I think the ‘intact perineum badge of honour’ extends to women themselves. I remember being so proud of myself for focusing, breathing and allowing myself to stetch and open, rather than just pushing hard and getting it over with. (I did feel like I was going to tear at the front, and instinctivly guarded myself, as I was adamant that I didn’t want a clitoral tear). I’m sure I would have seen myself as a ‘failure’ if I sustained more than the minor 1st degree tear that did. This is despite me knowing that this tissue, in being so similar to that of your mouth heals quickly and easily (as well as achieving the vbac I so desperately wanted!).
Thank you for this. I’d like to add not to blame the mother! I feel almost guilty for having torn, like if I’d only … I wouldn’t have. I appreciate the recognition that tearing is on the spectrum of normal and it’s not my fault.
Oh and my midwife ALWAYS asked if she could touch me, even when I was crowning and asked her for her help she repeated, “may I touch you and see where the baby is” – since I was in the pool and she couldn’t see. 🙂 <3
Such an important point Usha – tearing is NORMAL. Most women tear with their first baby regardless of what they do to avoid it. We are designed to tear and heal, it is all part of the process. No woman should blame herself for tearing – it was what her body needed to do to birth her baby – no shame in that. x
This is interesting and something I have thought about a lot. I was very stressed over tearing and wanted to avoid it. I tore with my first 3. My second child – 3rd degree tear and the others 2nd degree. I tried to avoid it with my third by breathing rather pushing. I think the stitches were harder to deal with than the tearing which I agree is normal. I think the positioning is most important too and water. I had my last baby (#4) in water and I didn’t tear and what a world of difference that was!
I was very stressed over tearing and wanted to avoid it.
I have learned about midwives in other cultures gently “pushing” the baby’s head back in the vagina as it’s descending, to allow the vaginal and perineal tissues to gradually stretch. Supposedly, they have very good outcomes with fewer perineal tears. An acquaintance of mine who is living in Japan (she’s American) gave birth recently with a midwife who did this. She described it as extending the 2nd stage by about 10 minutes, but she was incredibly grateful that she did not tear at all, esp. compared to her first birth where she had a large tear and long healing process. Just food for thought. 🙂
But I totally agree that too many providers assume they should just jump right in and give perineal support, without considering that it may be too intrusive on the woman. A woman’s autonomy and wishes needs to be respected, even if it means she risks tearing. And so wonderful that you pointed out the importance of reminding women that their perineums are not only designed to stretch, but also to tear and then heal!
I have seen midwives in the UK and Australia do this too to ‘prevent tearing’. It may or may not work. However, wouldn’t it be nice if the mothers felt empowerment and belief in themselves as the experts in their birth rather than feeling ‘grateful’ to the midwife. They may not have torn anyway and if they end up with a 3rd or 4th degree tear would they be ‘grateful’ – this hands on approach increases the risk of major tearing : )
Is the practice of ‘flexing the head?’ I remember as a student midwife being told that a woman had torn because I hadn’t flexed the head. I witnessed it again yesterday as a return to practice student and realised that I have never incorporated it into my practice, and didn’t ever feel as though I could make any difference either.
I would welcome any thoughts on this?
Wow – this is a very outdated practice. I found an article about it which I included in my thesis literature review. Basically it can increase the risk of perineal trauma. If you flex a direct OP baby’s head thinking it is OA you will deflex it increasing the presenting diameter. Even with an OA baby, the baby will find the path of least resistance and be guided by maternal tissues… and baby’s head are born by extension, so you are forcing them to go against physiology. Also I would be interested in consent was gained for this procedure? My thoughts on this are keep hands off women and babies as a default. And there is no research to support that anything you do as a midwife re. your hands will prevent a tear occuring.
I am a midwife with a homebirth practice and had worked for 17 years in hospital in a natural birthing center and have caught about 7000 babies over the last 33 years. I was taught to flex the head, have the woman breathe upon crowning, use hot compresses with oil. I never cut episiotomies unless there is severe fetal distress and need to get baby out quickly ( very very rare). About 30% of primips would tear, mostly 1st or second degree tears, some needing stitching. Since 1999 I have had my primips use the epi-no and my tear rate has decreased to about 13% and I use the same other techniques, warm compresses with oil, slow breathing out the head, and sometimes keeping the head flexed. I believe that it is important to flex the head because it will present a smaller diameter. Sometimes I have women that want total hands off, and they definately tear more often from my experience. However, I am positive that the epi-no is the determining factor in my lower tear rate. I also find that women tear more in waterbirths, maybe related to the hands off. I have had plenty of repeat births of the primips who have used the epi-no and find that there is no difference in their pelvic floor as far as being “stretched out”. In the beginning I also thought that I wouldn’t like the “invasiveness and articficiallity” of the device, but once I got over that prejudice, I see the results are amazing and it also shortens the second stage, and raises the confidence level of the woman. In short, I absolutely LOVE THE EPI-NO AND HIGHLY RECOMMEND IT.
I am sure the epi-no would reduce the chance of tearing… in the same way as perineal stretching (massage) does. My concerns about the epi-no are about long term effects to the perineal muscles (which are not stretched in ‘massage’). There has been no research – and probably will not be due to funding – about how these women’s pelvic floors function later in life (menopause) after effectively ‘giving birth’ multiple times to an epi-no device.
I have the opposite experience to you – I generally do nothing as the woman births her baby as a risk management strategy, and have not sutured a perineum in 7 years. Some tears but nothing significant. It is important for women to know that different practitioners have different approaches. As long as they are fully informed of their care providers approach and give consent to any interventions – informed by full disclose of the research evidence supporting that practice – then all is good. It really is about what the woman chooses and consents to. 🙂
just to add to your data collection 😉 I am 5’6 and started my 1st and 3rd pregnancies at around 220lbs and gained about 30lbs with each. Pregnancy in between I started at around 190lbs but gained 40lbs in pregnancy (nursing 1stborn really sucked the weight off me! wish #2 had been such an enthusiastic “extended” nurser but he was all business about it – wanted off as soon as he finished his meal part of the exchange, not a comfort nurser as he preferred a pacifier after having reflux issues).
I had a “would have taken one stitch” tear toward the front that made peeing uncomfortable for a few days after birthing my first. Did not do perineal stretching during pregnancy with any dilligence (I think we did a few times here and there). Labored in the tub for a few hours then had to get out to push (not sure if it was hospital-run-birth-center policy or due to midwife’s back pain, she also couldn’t catch him on a birthing stool and I know that was a pain issue for her). Sat on the edge of the bed with my back extremely arched (no way I could have caught him!), she applied warm wet washcloths to my perineum while I was pushing – can’t remember if she asked my consent before the putting on the first one but I was quite happy to have it there and remember panting out “please put one toward the front” while trying not to let my body push too hard. Tiny 1st degree tear going toward my clit (which, maybe TMI, but has actually turned out to be beneficial – before my first birth that area was too sensitive to be pleasurable during intercourse, stimulation would just make me feel like I needed to pee. Now that’s not a problem and it’s just the right amount of sensitive 😉 ). He crowned for about 15min then MW announced “I think the head is going to be born on the next push, Dad do you want to step around to catch your baby?” I yelled “DON’T MOVE YOUR HANDS!” and about 10 seconds later my son was on my stomach. Did not get a stitch, would have only taken one if I’d opted for it but didn’t want the extra distraction of being stitched up at that point. Baby was 8lbs 5oz with fat rolls at birth.
2nd birth was a home waterbirth with a traditional midwife side-lying (hubby & MW didn’t realize I was so close to birthing to start filling the pool soon enough, side-lying was my choice only because it was the only way to have water on my tailbone and belly at the same time and I was having back labor at the end, suspect he was posterior until he came out, he didn’t fully DROP until just before he was crowning). Whereas my first never floated back up after starting to crown and just kept crowning progressively more and more until he prtty much fell out whole in one contraction, my 2nd “turtled” – crowning then going back up – for about 30min and actually had his head born about 30 seconds before the rest of his body with a rest break in between (that feeling of baby’s head out and they’re turning and squirming is the WEIRDEST sensation!!!). No tear at all, could sit in Tailor Pose when he was hours old without discomfort. 7lbs 14oz at birth.
My 3rd (11wks old now) was also a home waterbirth. I would call my birth position “frog pose” – hands and knees but with butt REALLY low to the ground and knees spread wide. This was my comfort position through six weeks of prodromal labor (and then the little booger waited 10 days after his EDD – my first was born the day after his EDD and my second the day before, dates all arrived at via 1st trimester ultrasound done because of VERY irregular periods). I spent a lot more time in the water with this birth (wouldn’t let my husband completely drain it after the events of my 2nd birth!), I think I was in the pool with warm water being added starting about 3 hours before he was born (got in the pool less than an hour before my 2nd was born). I flipped positions a lot trying to get more comfortable as this was my first birth I would actually classify as “painful” instead of “really hard work to the point of moderate discomfort” like my first two (I have been in chronic pain since I was 10 years old so my definitions of pain vs discomfort may be quite different than other women)- this guy had his fist by his cheek as he came out. Not sure if I actually tore or if I knicked myself with my own fingernail, felt like I had a papercut off to the side (and felt like it was running paralell to my labia) in the same area I had been working on a myofascial trigger point while in transition. I didn’t realize that my body was pushing this time around until he crowned, and he crowned for 1/2 a contraction then his head was born and the next 1/2 contraction his whole body was out, so he went from crowning to born in under a minute from my estimation (haven’t watched the video to try to time it, not sure if it’s visible on the video anyway but I remember yelling out “OH GOD! THE BABY’S CROWNING!” because I’d had it in my head that I was only maybe 7cm dilated at that point! Apparently my midwife DID realize my body was pushing even tho I just thought I had gas, she had her gloves on in the pictures that her apprentice took). This baby was 9lbs and if that was a tear and not from my fingernails (which really needed trimming!) it was less of a tear than with my 1st, only stung for a few hours.
As I mentioned above, I live with chronic daily pain and have for 2/3rds of my life. I hernaited 2 lubmar discs (L4/L5 and L5/S1) less than two months before concieving my first, and that pain was WAY worse than anything in my 3 unmedicated births, and took me over a month to recover from in any meaningful way. That was why I was adament that I was going to do everything in my power to avoid a c-section. I didn’t want to have to be spending so much time and energy recovering from surgery while trying to take care of a newborn. Instead, I wound up very empowered and I am pretty much back to my normal non-pregnant levels of endurance and pain within hours of giving birth each time. I wouldn’t trade my quick recovery from births for any “maybe” benefits, the only way I’ll let anyone intervene in what my body is doing while birthing is if there is CLEAR evidence of need in order to prevent life-long disability or death for me or my baby. The chances of that are so tiny though when mom is “allowed” to listen to her body and follow its cues while birthing instead of having someone else tell her what she “should” be doing at each point!
Hi Rachel,
Interesting article. I’d like to see research done out of the experience I had during my internship in Jamaica where there is poor nutrition, very low socioeconomic status, wide range of maternal age and parity, etc. Out of the dozens of births (all in the standard lithotomy position and no perineal support given) that I attended as a student midwife, there was not one tear. The ages ranged from 15 to 35…one breech and one set of twins, too! The births all occur pretty much in the same manner with the midwife verbally managing the pushing stage and vigorous cord traction in 3rd stage.
This is interesting Karen as it goes against the available research evidence. Sounds similar to the care I encountered in Nauru except everyone got an episiotomy. Unfortunately there has been no research looking at women’s experience of these approaches which I actually think is more important than outcome. I personally would trade lithotomy and being verbally managed for a torn perineum and having control of my own birth. Some women may not, and most don’t get the choice : )
I’ve loved this article and the comments that follow. I wish there was more research conducted in developing countries in general. I have no evidence to support my thoughts but I have worked for short times in Kenya and India. i can’t comment on birth outcomes but I wonder if women’s lifestyles play a part. Many women in developing countries perform manual work inside the home; bending, squatting etc. Likely to be naturally stretching their perineum or changing its strength perhaps? In the developed world I would think more women have sedentary lifestyles that involve sitting at work, sitting for the commute and sitting in the evening. I’m generalising I realise, but it’s got me thinking if this plays a part too? Be good to have some further research…!
there is a tool that can help women prepare their pelvic floor for childbirth called the EPI-NO. It reduces the likelihood of tearing and assists in strengthening the muscles – it’s not just about an intact perineum but about protecting the pelvic floor and preventing pelvic floor dysfunction…
Kim – I have come across this tool and cared for a woman who used it (intact peri). While I am sure it is helpful for many women I do feel a little uncomfortable about it for a number of reasons: 1. it encourages women to look outside themselves for preparation for birth 2. it encourages ‘intact’ = better 3. I worry about the effect of essentially ‘giving birth’ a number of times at the end of the pregnancy when the device is at it’s biggest. I wonder if this is good long-term for the pelvic floor. 4. I think there is a benefit in women actually touching and stretching themselves with their own hands – being comfortable with your body and gaining confidence from how much stretch you can get can increase body-trust. I’d be interested to hear other’s thoughts/experiences.
“For first time mothers perineal stretching massage during pregnancy can reduce the chance of tearing.” I question this because it assumes that the tissues can be “too tight” naturally and need to be manually changed over time (i.e. nature made a mistake,) and also I am very skeptical that stretching the tissue makes it stretchier, rather than just stretched out. It also ignores the fact that what makes the tissues stretchy in birth (and sex for that matter) is hormonal release, which is absent when the “stretching massage” is done in pregnancy. In essence, when we tell women they should manually stretch their tissues before birth, we are really telling them that there is something wrong with their tissues and their body will not respond properly in birth. Women’s tissues of course often do *not* stretch sufficiently, but really how often is birth allowed to progress normally in this culture? It’s crucial that a kind of “birthal arousal” be allowed to take place — analogous to sexual arousal when having PIV sex. The vagina and perineum are made to stretch, but not if a woman is afraid, distracted, tense, and those hormones aren’t flowing. If a perineum isn’t stretching, that says to me not that a woman’s body is defective and she needs help, but that her environment is preventing her mind and body from going fully into birth mode.
As for “hands-on support” of the perineum — my guess is that this generally does more harm than good. For me, anyway, it was very distracting and unpleasant to have someone with her hands on me, or even just sitting between my legs and watching. It made me tense up, and I lost my focus and connection to what my body was doing. Relaxation is going to take place only in the presence of my own hands or a trusted lovers, not a clinical practitioner, no matter how sweet and nice she is.
Linda – thanks for adding this important information about environment and hormones (I missed it out). As for perineal massage… I do still tell women about it and often they ask. My statement that “For first time mothers perineal stretching massage during pregnancy can reduce the chance of tearing” is based on two research studies which I have now added in (full ref list in lit review link). I feel it is only fair to share this information with women if it has been found to reduce tearing. This can be presented in such a way that you are not saying they are ‘too tight’ or that they can makes themselves stretchier. I suggest it is a way of feeling the body prepare and getting used to the feeling of stretch in that area of the body. For eg. I recently cared for a woman having a vbac. She wanted to do peri massage and found that she was able to feel effects of hormones as the pregnancy progressed and feel how much more stretchy she became. This gave her confidence in her body’s ability to prepare for birth and stretch during birth… which it did. For her this was positive. I also think that even in the best environment a tear can happen and that is normal.
Thanks for the article. I agree that many women tear or do not tear seemingly unrelated to whatever efforts are made or not made to prevent it. I have had primiparous women completely unassisted having completely intact perineums with huge babies, and similar women with small babies having massive tears out into the pelvic sidewall.
I can’t say I agree that one should just let tears heal on their own. All tears will eventually heal, but there are anatomical structures that are disrupted that will no longer be where they are supposed to be, particular with deeper tears. Leaving the posterior vagina torn open will definitely contribute to pelvic prolapse in the future, as it increases the side of the vaginal outlet – imagine two tubes – one with a large diameter and one with a small diameter – which one is easier to turn inside out? In cases of third degree lacerations, failing to repair the sphincter will contribute to incontinence of feces. There are plenty of folks in third world countries that can tell you about what it is like to live with a fourth degree tear that wasn’t repaired.
Small superficial lacerations that aren’t bleeding a great deal and don’t go through pelvic musculature are one thing. Tears through the posterior vagina that disrupt the rectovaginal septum or bulbocavernosus muscles should be repaired.
Any injury that doesn’t kill you will eventually heal, but that doesn’t mean that that natural healing process is superior or preferable to a correct repair. Correct repair of damaged anatomy is important for return of normal function, wherever that damage may be.
Hi Nicholas – thanks for checking out my blog. I’m not advocating no suturing so I hope it doesn’t come across that way. I might do a future post on perineal repair. When considering suturing I take into account whether there is bleeding (ie. a vessel that needs tying off), whether the perineal tissue is well aligned and how deep the tear is. I used to suture every 2nd degree tear until I began caring for women long term ie up to and beyond 6 weeks and saw how well they healed without sutures… and saw them birth subsequent babies. I now suture far less and find at homebirths women rarely have posterior vaginal wall tears, they usually get labial lacerations or nothing at all. As for third degree tears… these are NOT normal and are outside the scope of the midwife. I would want a surgical repair of a 3rd degree or 4th degree tear and suggest transfer to obstetric care for this. I do think the natural healing process is superior (and less painful) for most small, well aligned vaginal wall tears.
Im really surprised by this article. Ive never heard of any of these ideas. I got a 3rd degree tear and I never heard any of the nurses saying the midwife failed or I failed. Im pretty sure when it comes to tears it the luck of the draw.I had a big baby and I had a near fatal pph from a tear on my cervix. I lost 2 litres of blood. So these days the tear seems so minor. I learnt all about perineal massage from the ante natal classes. I was pretty worried about it. I even feel positive about all my battle scars from giving birth.
thank you for the insight on the culture of perineum.
my comment regards physiological pushing, really, as it relates to tearing. my experience is that, when women are not expecting to push with all their might, but simply let their body be the guide, tearing is less likely to happen. why? because they do not “push”, as there is no need. the body does it. and the natural sensations protect a mother from creating extra pressure by pushing. birth is not a race, and babies do not need to shoot out. most of the time, there is no urgency, contrary to what our media tells us: baby is connected via umbilical cord, and is well able to adapt to the reduction of oxygen during contractions.
pamela hines-powell has great information regarding the perineum and a “hands-off” approach. here’s a link: http://aamishop.com/index.php?main_page=product_info&products_id=140
blessings
another wonderful, thought provoking post that I thoroughly enjoyed. Thanks! The salient points for me were:
1. I formed the view a while ago that if a lot of women experience tearing (in all sorts of birhting environments, and from various ethnic/cultural groups) then perhaps it’s physiological rather than pathological – albeit unpleasant and uncomfortable (like diarrhoea or vomiting in labour)- and in fat we need to reframe our attitide. Perhaps, even, it is actually an important factor in a great and complex system that means that a new (commonly 1st time) mother is less mobile: to ensure she rests/recovers, gets support from others while she focuses intensely on her new baby for a shortish period of time. I like Delightfulbirth’s comment “…reminding women that their perineums are not only designed to stretch, but also to tear and then heal” this approach normalises the experience so noone feels a failure when it (inevitably) happens. Interestingly it happens much less with subsequent babies when the mother may eed to be more mobile earlierto care for other children.
2. increasing reliance on yet another technolgy, rather than reflection and appreciation of basic physiology/endocrinology to reassure us that the perineum WILL stretch. i.e the increasing levels of relaxin during pregnancy, peaking in labour to facilitate pelvic and soft tissue stretching, and interestingly to diminish uterine contraction…maybe women aren’t MEANT to push too forcefully as the baby’s birth approaches. For me, there is a HUGE difference between perineal massage with one’s own (or partner’s) fingers and using a device designed to change our anatomy…one is about self-exploration, undertanding our own anatomy and finding ways to work with our own resources and strengths, the other is moving the locus of control away from ourselves, to something external that is percieved as superior to our own inate knowledge – like the dating scan that “proves” a woman is pregnant and due on a certain date, regardless of her already being sure becasue she knows her cycle and her body .
3. your reminder that legs/knees together actually takes pressure off the perineum and helps rather than hinders the birth. My lighbulb moment was “of course, the baby’s head has emerged throught the pelvic outlet by that stage so a wide, open position is not as necessy as previously, when she/he is navigating the spaces withing the pelvis”
Simply wonderful stuff!
Maxine
“It is also a reflection of our technocratic culture that a ‘device’ is considered to be necessary in order to prepare for childbirth.”
I must admit that I am actually a huge fan of the Epi-No and considering it was created from an African tradition of using a calabash in a similar way, I don’t think it is entirely true to say it is a reflection of a technocratic culture. I would, however, say that if a woman is using it thinking it’s a magical pill to avoid tears then that is another thing all together. The reason I, and many others around me, advocate its use is that it helps women (either first time mothers or those who had difficult previous experiences) to build confidence in their bodies. We encourage them to use it to locate the muscles they will use to push the baby out, thus building confidence in their own intuition.
I think so long as one is promoting it’s use from the perspective of letting a women get in touch with her body and build confidence in its ability to stretch and heal, then it can be a very positive tool for her to have access to. It doesn’t need to be about obsessively working towards not tearing.
Anything that helps a woman build confidence in her body is good. I can see it could allow women to get familiar with the intense sensations of birthing. Not sure about encouraging them to locate the muscles they will use to push the baby out. I’d be careful about implying that ‘pushing’ is anything but involuntary and instinctive. It reminds me a little of a research study into teaching women how to push ‘effectively’ antenatally so they could perform well during birth. I have have an awful image of women ‘practicing’ pushing by putting a huge balloon into their vagina (essentially what the epi-no is) and commencing valsalva pushing ‘long an hard, into your bottom’ with a stop watch 😮
OK now I’m getting carried away 🙂
I agree that no-one could have possibly taught me to push, because it wasn’t “me” pushing. My body completely took over the job and I was just a vessel for my bodies instinct.
But I agree that if a woman feels like she needs to “do” something to help her prepare then fair enough. I had an epi-no in my cupboard that I never touched prior to my hbac. I thought about it cos I had used in in my first pregnancy. This time however I focused my attention not on preparing my body persay but in just supporting my body to be healthy so it could do the job it was designed to do. So I never touched the epi-no. I just remeinded myself to trust in my body. Each woman is different tho and what works for some may not work for others
Women don’t practice pushing with the epi-no. It is just a stretching device where they work at their own individual pace and it actually really enhances their confidence in their bodies ability to stretch and familiarizes them with the stretching sensations so their fear is lessened also. Ilana
Well that is not what women are being told to do with the device by the people who are selling it. I think it is great if women gain confidence by using the device. It would also be good if they had full information about perineal health, stretching, healing and the risk of epi-no. In Queensland the state guideline on perineal care states the concerns clearly – women should have this information.
The instruction manual does not say to “push it out” or practice pushing. It is written:
“At the end of the stretch, relax your pelvic floor muscles and allow the balloon to gently expel itself from the vagina. This simulation of birth allows you to experience the sensation of birth ahead of time. “
Maybe women are misinterpreting “Following the stretching exercises the balloon can be glided out, simulating the experience of control during delivery”. The idea of ‘control’ during delivery being assumed to be actively expelling.
Not sure where you are registered but in Australia there are clear standards from NMBA (registration body) regarding promoting products to clients. Along with the law relating to information sharing and government publications outlining concerns with the product – I’d be wary of recommending an epi-no to clients. I have looked after a women who used one but she made an informed decision with no recommendations from me.
So in Australia you are not allowed to recommend a product if you think it is beneficial to your client? Like taking an iron supplement or buying a support stocking for varicose veins or a breast pump or getting an epi-no? Here in Israel we do not have such a law. We can recommend and of course the client makes the decision to buy or not.
In Australia we have a professional and legal obligation to provide adequate information regarding an recommended intervention. We can recommend interventions that are evidence based ie. iron supplementation etc. We cannot recommend a specific device when there is a better alternative (digital perineal stretching) with a better evidence base. We cannot step over the line of marketing a device for a company’s profit. Of course women have the freedom to choose to pay for such devices if they wish – but it would be unethical and unprofessional for me recommend it.
In the research done with Epi-no, it was compared to a group that did perineal massage and the results of the epi-no were much better. This has also been my experience. From 1083-1999 all my primips did perineal massage. From 1999 to present, they mostly use the epi-no, and my rate of tears has dropped tremendously. I am convinced that it is due to the Epi-no. The rest of the techniques are the same and I am the same provider.
Practise is generally experience and belief based and we tend to reinforce our belief systems by looking for experiences and evidence that fit. I am not going to continue arguing the evidence – I think the guideline I linked to provides a good summary of it. I will continue to promote women’s belief in their body’s innate ability to birth and mother – it seems to work well for the women I provide care for 🙂
totally agree – this is what i teach.
Well I know that that wasn’t me you referred to in your article, because it was written before I birthed my baby, but I find it funny, that I am not the only woman to want to push her own baby back in whilst it was crowning 😛
It was written before you birthed but updated and edited today 😉
Oh well in that case Pmsl!!!! That was such an irrational and totally instinctive out of control moment! When you come for a visit we can watch my video, it is terribly funny and beautiful in turns :). I must admit I have laughed a lot watching her crown. I think I had completely lost the plot at that point and it was touchingly raw and honest and hilarious all in one 🙂
You are supposed to lost the plot. Your body and instincts need to overtake any logic… and the effects are funny sometimes 🙂 Can’t wait to see the video! x
VERY good article! I agree in theory about your comments on the EPI-NO… it’s actually a product that I carry in the pharmacy I work at when not attending births. I think the advantage is, giving women who are NOT already trusting of their own bodies a way to practice feeling and experiencing sensation in that area can help instll confidence that their bodies ARE capable of stretching and birthing baby. I’m in favour of anything that teaches women who have been taught by our current birth culture that their bodies aren’t capable of birthing their babies that they CAN in fact do it!
That being said, the other tips in hear are amazing and need to be spread around! Sharing!
VERY good article! I agree in theory about your comments on the EPI-NO… it’s actually a product that I carry in the pharmacy I work at when not attending births. I think the advantage is, giving women who are NOT already trusting of their own bodies a way to practice feeling and experiencing sensation in that area can help instll confidence that their bodies ARE capable of stretching and birthing baby. I’m in favour of anything that teaches women who have been taught by our current birth culture that their bodies aren’t capable of birthing their babies that they CAN in fact do it!
That being said, the other tips in hear are amazing and need to be spread around! Sharing!
As a sexologist I have to agree with your reluctance to endorse the Epi-no. I’ve had several clients who have used this device and then had to use vaginal weights post natally due to overstretching, which inhibited their pleasure and that of their partner. I’m sure that this issue isnt paramount in a birthing mother’s mind at the time of birthing :), but should be a consideration none the less.
Thanks Emma – That’s interesting and an assessment of long term ‘side effects’ should be included in any research about the effectiveness of the device.
You have no way of knowing that this was a result of the epi-no, but rather of the birth itself. A study was done to assess pelvic floor function after six months comparing a group that used the epi -no and a group that didn’t, and it was a blind study, and no difference was found between the two groups. Also, the epi-no Delphine Plus model is used after the birth (from cessastion of bleeding) to do pelvic floor strenthening exercises (without inflating) and should benefit after birth pelvic floor function.
Who was the study funded by? Epi-no? I’m interested in longer term outcomes ie. menopause.
The Effect of the Pelvic Floor Training Device Epi-No® on the Maternal Pelvic Floor Function Six Months After Childbirth – Follow-Up Study of a Randomised Controlled Trial
C. Dannecker, C. Baur, E. Ruckhäberle, U. Peschers, K. Jundt, A. Reich, M. Bäuerle, K. T. M. Schneider
1 Klinikum der Universität München, Klinik und Poliklinik für Frauenheilkunde und Geburtshilfe – Großhadern, München
2 Frauenklinik und Poliklinik der TU München, Klinikum rechts der Isar, München
3 Frauenklinik Dachau
4 Klinikum der Universität München, Klinik und Poliklinik für Frauenheilkunde und Geburtshilfe – Maistraße, München
5 Universitätsfrauenklinik Ulm
Abstract
Purpose: The aim of this study was to evaluate the effect of a training with the pelvic floor training device Epi-No® performed during pregnancy on maternal pelvic floor function six months after childbirth.
Material and Methods: This is a follow-up study of a randomised controlled trial (recruiting period between 2/2000 and 2/2002). Pregnant nulliparous women were invited to participate in this study and – if assigned to the study group – to practise daily with the pelvic floor training device Epi-No® from 37 weeks of gestation on. After childbirth all women from one of the recruiting centres were scheduled for evaluation of the pelvic floor function by a comprehensive examination, including the following techniques: questionnaire (urogynaecological symptoms such as stress incontinence, overactive bladder, anal incontinence etc.), pelvic floor muscle strength (Oxford score), anal manometry, endoanal sonography and introital sonography.
Results: 146 women of one centre represent the collective of this study. The return rates of the questionnaires (before and after delivery) were about 84 %. Follow-up was performed at 7.4 months (mean) after delivery and was possible for about 76 % of women. With regard to important obstetric variables there was no difference between the study and the control groups. The same applies to the questionnaire data after delivery (at the time of follow-up examination). We found no significant differences with regard to bladder neck mobility (introital sonography), incidence of occult anal sphincter trauma (endoanal sonography) or with regard to anal pressures at rest or during squeezing and for the maximum pelvic floor contraction strength (Oxford score).
Conclusion: Training during pregnancy with the pelvic floor device neither impairs nor substantially protects pelvic floor function at 6 to 8 months after childbirth.
That is one very small study and when evaluating an intervention you need to look at all the available research. Queensland Health guidelines provide an overview/summary of all of the current research. You can download the full document and references here: https://www.health.qld.gov.au/qcg/html/publications.asp#maternity
Cut an paste of the summary:
PERINEAL STRETCHING DEVICES
Risks/Benefits:
Three studies40-42 involving primiparous/primigravidae women show the device:
• May be associated with bleeding, pain, contractions and dislocation of the balloon device in the vagina during training
• Is not associated with vaginal infection if hygiene instructions are followed40
• Injury incidence – reduces the likelihood of an episiotomy in high episiotomy-use settings40,41
• Increases the incidence of intact perineum40,42 not fully explained by a reduction in episiotomy rate
o Does not consistently affect the overall rate of perineal tearing40-42
• Possibly may reduce severity of perineal trauma41 (very small study,
n=32)
• Has no observed negative influence on the pelvic floor (i.e. bladder neck mobility, pelvic floor contraction strength)40
Recommendation
• There is insufficient high quality evidence to promote the general use of this stretching device
• Encourage women to continue to perform perineal digital massage and PFME
Yes it is a smalll study. However, if you think that about 30% of women first births will tear, do you know what long term effect this will have on the perineum? Has this been researched? It seems to me just logically that there is more damage with tears and sutures than with using an epi-no and an intact perineum.
I do talk about perineal massage with my doula clients, and I’ve used it myself. I had a spontaneous 4th degree tear during the home water birth of my daughter, and I’ve never quite figured out why. The term ‘dysfunctional perineum’ was mentioned a couple of times, so I’m guessing my perineum is quite short.
Post natally it took me a long time to recover from the tear and subsequent surgery. However, I am still very tempted to give vaginal birth another shot if I’m ever fortunate enough to have another baby. xx
what an awful term ‘dysfunctional perineum’! There are some physical differences between perineums and some are ‘shorter’ than others = less tissue to stretch. I hope you have healed well x
A really interesting read, thank you. Particularly liked the reference to positions which don’t overstretch the perineum – will add that to my teaching.
I’d always assumed that women from cultures where squatting is the norm in daily life are less likely to tear, as the perineum is more elastic from use than those of us who sit cross legged at computer terminals all day (just realised that’s what I’m doing!). Would be interested to see if this is the reason the Jamaican women had less problems.
My own first birth sustained 2nd degree in left lateral, and second birth another 2nd degree kneeling (breech). However, 2nd time healing was much more comfortable, which I put down to the IM suturing the muscle and leaving the skin. I’ve never heard of anyone else doing that, so don’t know how common it is.
Regular squatting alters the physiology of the pelvic floor, making it much stronger. Kegel/pelvic floor exercises are not so good. More info here:(http://mamasweat.blogspot.com.au/2010/05/pelvic-floor-party-kegels-are-not.html). I think the theory behind differences in tearing between ethnic groups is to do with the length of the perineum. However, it would be more interesting to look at outcomes according to birth place – all of the studies were or women birthing in a western, technological culture.
It is often recommended to leave the skin when suturing because it is the skin that hurts the most and causes the most problems healing. I would not generally suture skin 🙂
Hi Rachel,
Thanks for the great post, especially the excellent list of references.
I have a few comments…
First, check out the Mama Sweat blog followup that says kegels ARE invited to the pelvic floor party (and follow links to more info from Katy Bowman and me):
http://mamasweat.blogspot.com/2011/06/second-annual-pelvic-floor-party-kegels.html
Yes, an overly tight pelvic floor is bad news! But good kegel technique provides phenomenal benefits while allowing the PF to remain supple and stretchable — like any healthy skeletal muscles.
Just so you know where I’m coming from, I’m a homebirth mom, former doula & CBE, & onetime student midwife. I am TOTALLY on board with care that supports women in physiologic birth and intervenes only when it’s really and truly indicated.
The thought that perineal tears are best considered part of the spectrum of “normal”/physiologic birth is provocative. I’m not sure whether or not I agree. Tearing is common, but is it helpful for us to consider it normal? Sure, it’s helpful to remove any stigma of failure on the part of the woman or midwife. But what is “normal,” anyway? Even the most instinctive, least-interfered-with birth is still happening within the context of a woman’s culture and physiology, both of which are heavily influenced by numberless and enormous departures from the hunter-gatherer context our bodies evolved for. How many Paleolithic women had perineal tears at birth? I don’t know. I would love to see some research that attempts to answer that question.
Another thing that is prominently in my mind as I read this article & the comments is that preventing tears is only one part of preserving the health of the perineum. Many women suffer with pelvic floor problems after childbearing even without tears. It may be useful to expand the conversation to focus on optimizing perineal and pelvic floor health.
With that — and my experience with thousands of women suffering with prolapse and incontinence — in mind, the epi-no sounds like a recipe for pelvic floor damage and the potentially hellish problems that can result from that. I used perineal massage in my 3rd trimester (I have just one child). That was ever so gentle encouragement to release tension in the muscles, not “let’s practice massively stretching over and over.” (And BTW, I believe the perineal massage helped me give birth with nothing more than a couple skid marks, even though my daughter’s hand came out next to her temple.) The epi-no may have been inspired by traditional birth preparation practices, but let’s remember, a lot of traditional cultures do non-physiologic things like withholding colostrum (and for heaven’s sake, FGM). I totally agree, Rachel, with all your concerns about the epi-no.
Thanks again for a great post & great dialogue,
Alyce Adams, RN
The Kegel Queen
Pingback: Episiotomies… Tear Here —> | Esali Birth Blog
Hi Alyce – thanks for your comments. It is great to have input from an expert in the area of the PF. I have a few responses/questions:
“The thought that perineal tears are best considered part of the spectrum of “normal”/physiologic birth is provocative.”
Two thirds of women sustain perineal tearing/lacerations/grazing during birth. So statistically it is very normal. Even in the context of an undisturbed, instinctive birth (the majority of births I attend) there is usually some ‘trauma’ to the soft tissues for primps… although not usually enough to require suturing.
“…influenced by numberless and enormous departures from the hunter-gatherer context our bodies evolved for. How many Paleolithic women had perineal tears at birth?”
I am totally on board with the Paleo perspective, I eat and exercise ‘paleo’ and know personally how life changing it is to do what your body evolved to do. I would also love to know about tears for Paleolithic women. They certainly ate a better diet and probably spent time moving and squatting in ways that modern woman does not. I am pretty sure they did not do Kegels. However I think they still would have encountered tissue damage to some extent… other mammals do. The minor damage and swelling would have ensured that they curtailed physical activity, rested and focussed on their baby. All totally theoretical of course!
“Many women suffer with pelvic floor problems after childbearing even without tears. It may be useful to expand the conversation to focus on optimizing perineal and pelvic floor health.”
I would be way out of my depth heading into this area… there are people such as your self doing this with much greater knowledge than I have. My posts stick to what I know and therefore will never cover all dimensions of every topic I discuss.
“The epi-no may have been inspired by traditional birth preparation practices, but let’s remember, a lot of traditional cultures do non-physiologic things like withholding colostrum (and for heaven’s sake, FGM).”
Totally agree. Just because a practice is traditional does not mean it supports physiology. There are some horrific traditional practices that midwives carry out/have carried out globally and historically.
Thanks for contributing to the discussion 🙂
To be honest I totally panicked when it came to pushing and it wasn’t the OMG there a baby coming out that freaked me out but the lithotomy position, having utterly no control, feeling pinned down by the family and the nurses (husband and MIL on either side holding my hands and nurses holding my legs in the stirrups), being screamed at by everyone to push and *the ultimate thing that made me freak out was the ‘hands on’ approach the Nurse-Midwife had with my vulva.*
I have had many sexually traumatizing moment in my life but that one takes the cake, she never told me she would be ‘hands on’, she never asked for my permission to touch me and with wave after wave of contractions bearing down upon me I couldn’t speak to tell her to STOP touching me. I couldn’t even kick her hands away which I did try to do but couldn’t, damn those nurse holding my legs in the stirrups!
Left alone and with a hands off technique I know I would not have panicked, I was completely confident in my ability to birth my daughter. Instead I was left with a lateral labial tear and yet another traumatizing event I have yet to recover from.
Midwives please if your patient/client is a sexual assault/rape survivor please, please, please talk to her about the approach you will take with her vulva, make sure that ‘hands on’ approach is okay before you jump in and ‘guard her perineum’ the whole time, otherwise you may just re-traumatize her.
Ps – Please do a post about lateral tearing, I would love to hear what you have to say about it. There just isn’t enough in depth info out there on it, it’s given a very cursory, glossing over at best.
And as many women will not reveal previous sexual trauma, and because what you describe would be traumatic for anyone, let’s have that nice hands off approach, asking permission if necessary to touch, and full discussion, for ALL women.
I agree Kathryn. All women regardless of their previous experiences should be treated with respect. That includes not touching her genitals without very good reason and only with consent. It amazes me that once a woman is in labour all social and cultural norms are suspended and people are quite happy to touch her genitals in the most ‘everyday’ manner. Also 1 in 4 women have experienced sexual abuse/trauma and not every woman wants to tell her midwife (which is fine). Unfortunately many women suffer abuse and trauma from their insensitive care during labour.
As for lateral labial tearing… In my experience this a common occurrence, especially when women are on all fours.The labia seem almost ‘designed’ to take up the stretch during birth and do a great job of it. Vaginal wall tears are more common in supine positions. Usually labial tears are just a graze or minor tear that heals itself. Sometimes the labial are torn in two and can be sutured for cosmetic effect or left without problems. I am sorry you had an awful experience 🙁
Agreed. The OB doing unwanted perineal fanning without warning was the worst and most painful part of my first birth. I think some OBs forget when a woman doesn’t have an Epidural can feel what they’re doing, but they should ask regardless.
I’d like to ask some advice if that’s ok, I recently had a homebirth VBAC and had a second degree tear that went up a couple of centimeters into my vagina (the posterior wall I guess you’d call it). My midwife said that it would most likely heal quicker if it was stitched and so I went ahead with it, now, 2 months PP, there is a tight band of scar tissue on my perineum which is uncomfortable to stretch for sex, let alone having another baby.. So my question is, after a decent tear with a build up of scar tissue, will I tear again during any future births?
Thanks in advance for your thoughts,
Cindy
Scar tissue is not as ‘stretchy’ as non-scar tissue. Often women will tear along a scar line but not usually badly. In your case it may ‘release’ some of the tightness for you. You could try perineal massage with lots of oil. Vitamin E oil is good for scars, but any oil will help with massage. Have a look at Carolyn Hastie’s instruction leaflet (link in the post). You don’t have to wait until you are pregnant to try and stretch your scar tissue. Good luck 🙂
Pingback: Birth Sensations & Protecting The Perineum Through It All | The Joy of This
Hi I am not pregnant, never been pregnant nor am I ttc. I am just learning more about my body so if one day it ever happens I am well armed. I have PCOS and with recent weight loss I have had 4 periods since December which is great because they were absent for 3 years. Is it possible, I mean do you know of women who have gotten pregnant with PCOS?
Secondly with this post I wanted to ask about perineal skin. I have a lot of excess skin in this area, I mean skin you can get a good pinch of. I was considering excising it surgical fir aesthetic reasons? Would this make me more likely to tear during birthing? Thank you and thank you for this amazing blog!
Oubli said…
I read on a L&D blog written by an RN that these types of surgeries creates massive scar tissue along with an aesthetically pleasing look, because scar tissue does not have the same capacity to stretch the tissue literally SHREDS as the baby is being born.
So all the ladies out there looking at having these types of procedures done should ONLY have them done AFTER they done childbearing or if they are a C-Section Only Lady.
This is the reason why I haven’t yet had my labia minora repaired, it split horizontally during the birth of my daughter and healed up into two separate pieces because of an inept stitching from my midwife. Since I read that RN’s experience I have had visions of my next birth where I am shredded to pieces if I get that repaired. The repair will be done when I am done childbearing.
Anonymous said…
Report: Vaginal Plastic Surgery Has Same Risks As FGM
The real kicker of the report, though, is its examination of the risks involved in labioplasty. The authors mention a potential loss of sexual sensation, which we’ve heard before. But they also say that the procedure may cause some of the same childbirth problems as female genital mutilation does, including bleeding and tearing in labor, and even the death of the infant. Anyone eating breakfast might want to skip this part, but a commenter on a an earlier post shared some first-hand experience with the problem:
In nursing school I helped out at the delivery of a woman who’d had labiaplasty several years before, and holy shit. It sort of, um, shredded. One of the most horrific things I’ve seen in my career. It took them a really long time to sew everything back together, and I have a feeling she would have happily gone back to some slightly asymmetric or (gasp!) flappy labia if she could have.
http://jezebel.com/5402091/report-vaginal-plastic-surgery-has-same-risks-as-fgm
http://mitchsmom.blogspot.com/2012/08/labiaplasties-gyn-alarmed-what-your.html
http://mitchsmom.blogspot.com/2012/08/labiaplasties-gyn-alarmed-what-your.html
I totally agree with Oubli. I have seen a lot of female genitals. Most women have labia minora that protrude out from the labia majora… and enough to ‘pinch’ (ouch). The labia minora have an important function during sex (tugging on the clitoral hood during intercourse) and during birth (providing enough skin to stretch and allow the baby’s head to come out – usually without tearing). In some cultures young women are encouraged to regularly stretch their labia minor… the longer the better!
In our culture regulations about ‘indecency’ have determined that labia minora cannot be shown in photographs… neither can erect penises. So, ‘adult’ models are selected for small labia and any bits sticking out are airbrushed away to meet the regulations.
I have often wondered what would happen to labia that had been ‘trimmed’ during birth and Oubli has answered that question – and I am not surprised considering how much the labia stretch during birth.
As for PCOS – yes, I know women who have got pregnant and had babies despite having PCOS… it sounds like you are getting your fertility back. Good luck 🙂
Aw, this was a very good post. Taking a few minutes and actual
effort to make a good article… but what can I say… I hesitate a whole lot
and don’t manage to get anything done.
Pingback: Cris Doula Acompanhamento na Gestação, Parto e Pós-parto! » Como evitar lacerações no parto?
Thank you again midwifethinking for such a well-thought out, balanced, and comprehensive article. You never disappoint. I so appreciate your work.
Thank you. I appreciate your work too 🙂
This really is a great blog! I find checking for tears after birth a very uncomfortable unpleasant experience for most women. What are the thoughts on checking the cervix after birth in the absence of heavy bleeding? Often just checking the vagina causes a lot of discomfort and I am being as gentle as I can be. Do you think it’s necessary to visualize the cervix/high vaginal walls after childbirth if bleeding is not heavy? To me it often feels unnecessary and very invasive for the woman.
My thoughts on routine checking of the cervix = that it is unnecessary and barbaric. I’ll take the extremely small risk that there is a significant tear that is somehow not bleeding, that I miss because I did not carry out this procedure.
Pingback: Did You Know? (15 Oct 2013) | Williamsburg Mothering
Hi Rachel and others,
Im after comments on clitoral tears and peri urethral tears, healing and what women may expect to experience when resuming love making, or is it really individual. Does the clitoral area have the healing benefits like the vagina…..Thanks.
Hi Sally – I don’t have a lot of experience of this type of tear (luckily!). Hopefully others will comment. I would imagine that it would be individual. The clitoral area has a rich nerve supply so there may need to be some nerve healing too.
Tearing doesn’t normally happen through the clitoris but around it these are normally shallow but very, very rarely can run deep, tearing through the clitoris just doesn’t happen because the tear will choose the path of least resistance and that is not directly through the clitoris. Clitoral tears will take extra time to heal and require extra care to keep clean from urine. Adhesions can happen also, this is where the tear heals grafting itself onto surrounding tissues. Watch out for this and be prepared for you or your care provider to prevent this from happening by carefully apply anti-biotic/petroleum jelly (I suggest comfrey/marshmallow salve with anti-biotic herbal properties) to keep the torn clitoral hood healing/adhering to the clitoris itself. Peri-uerthal tears are usually micro tears aka spider (web) tears which are irritating, burn during urination, cause urethal swelling and extreme pain/discomfort from said swelling but again urethral tears through the urethra don’t happen – they are so very, very rare – path of least resistance and all. The exception here is women who have had female circumcision or female genital mutilation, they may tear oddly, unexpectedly and in places that just isn’t normal because of previous incisions/scar tissue will offer the path of least resistance that intact women do not have.
Totally have the research on this down pat since there is virtually NO info on my horizontal labial tear, I went on a hunt for years on ALL info about odd tearing circumstances during childbirth ie searched for little known case studies, medical journal studies/trials, contacted doctors, talked to nurses and midwives alike.
Thanks Oubi – lots of great info there 🙂
Thank you for taking the time to respond Oubli! Sally.
It’s been 2 weeks since the home water birth of my son. I did everything I could to have a gentle birth but still sustained a ‘neat’ 2nd degree tear straight downwards. My midwife said we could suture it or leave it, and that it would likely heal well if we left it be. I chose to let it heal naturally but now I am so paranoid about it and scared that it wont heal properly and the skin wont come back together, and that I’ll have this big gap from my vagina to my anus. I’d love to hear any reassurance about 2nd degree tears healing without stitches.. I’m worried 🙁
You can find a summary and link to a Cochrane review about suturing vs not suturing 2nd degree tears in the post. It can take longer to heal unsutured but by 6 weeks there is no difference between sutured and non-sutured. Can you ask your midwife to have a look for you and reassure you that your tear is healing?
Please dont knock the Epi -no. It is a fantastic device and training only need take place once in the first pregnancy from 36 wks daily until the birth. It reduces pelvic floor trauma, reduces long 2nd stage, increases the mothers confidence and does no harm. If I could give it away to every pregnant woman, I would. It is expensive unfortunately. Hundreds of my clients have used it and it definitely makes a noticeable difference, makes my task alot easier as I suture less and is less invasive than manual perineal stretching. Regards
Marianne Littlejohn
I so agree with you.
Interesting article, thank you. A couple of thoughts…
Firstly, I was shocked to see the reference to socioeconomic status influence tear severity! This is something I have never heard about. Would someone mind explaining how this is the case? Is it related to induction? Do wealthier women choose to have more inductions? Or is this related to an the effect of having to pay for medical interventions in the US?
Secondly, having suffered from a 3c tear in my first labour, I’ve become consumed by this topic and carried out my own study into recurrence rates and causes. Not very scientific but some of your readers may be interested in the results. I’ve been blogging here: http://3rd4thdegreetear.wordpress.com
socioeconomic status is probably a factor because ‘private obstetric care’ is a factor… and women with more money are more likely to birth in the private system and undergo the increased interventions associated with this option.
Thank you for the link to your blog post – very interesting 🙂
Pingback: Protecting the Perineum – Paleo OB
Found this today after the difficult day at hospital as a student midwife. You are the breath of fresh air, my soul is resting, love your blog!
I would add another point to the preparation bit. Inspired by my own experiences and Ina May’s guide to childbirth. As I understand, the ability of our vaginas to stretch depends on tension – if it is very tense, it does not stretch and it hurts. For example, at tender age of 15 it might be difficult and even painful even to insert a tampon. The vaginal examination might be very painful for this reason as well. The intercourse can be very painful if the woman is frightened and tense and can even cause tears, especially if forced upon. One of the reasons for the fear is the lack of knowledge how big and stretchy we can get inside. Our vaginas are inside, invisible “folded” and as we grow up we are mainly unaware how spacious they can be. A thought of a baby’s head going through would be terrifying and when it is starting to stretch you feel you are tearing apart. Just awareness of our innate ability to stretch when we relax down below, the understanding can reduce the fear and tension and might also help avoid the tear. Ina May illustrated it by a story of a woman telling herself during birth “I am huuge” and then stretching really well. She also had an image of a stone figure in her book as a quite a powerful illustration of this point.
I agree… the vagina is a ‘potential space’ and tension can reduce how long it takes to stretch. I didn’t include this in the post because for some women it is impossible not to be scared and tense as a baby’s head stretches their vagina. I don’t want women to get fixated on having to feel a particular way during birth for it to work ie. relaxed. Birth works anyway regardless of fear or tension. Fear is usually part of the birth process: http://midwifethinking.com/2013/03/27/feel-the-fear-and-birth-anyway/ 🙂
Thank you for this article. I am eight months pregnant and trying to figure out how to best avoid serious tears and unnecessary procedures during my labor and delivery. I have read that perineal massaging in the weeks prior to pregnancy can help too, but my doctor told me that could lead to permanent stretching. Do you have any thoughts on this?
Also, while I like the empowering idea that women and their bodies have the instinctive ability to know what’s best for the birth, I also have to question that somewhat give that modern practices and science have so greatly reduced the risk of death for mothers and babies.
There is no evidence that perineal massage leads to permanent stretching… and evidence that it reduces the chance of tearing for first time mothers.
Medicine has reduced the risk of death for mothers and babies – it provides interventions for when physiology turns into pathology. For the vast majority of mothers birth is (could be) a physiological process. We are lucky enough in many parts of the world to have medical back up if birth becomes pathological. In the Western world the pendulum has swung too far and the overuse of intervention is causing many complications. MOST women have medical intervention during birth. Also, instinct and needing medical help are not two separate things. Women can instinctively know that their birth is ‘not right’ and that they need help. I always listen to this instinct.
A good care provider facilitates an environment that supports physiology and instinct… and notices when birth is becoming complicated… and accesses medical intervention WHEN necessary, not as routine. There is very clear research evidence to link medical intervention with perineal tearing.
Best perineal protection is to use Epi-no to stretch before birth. I am a homebirth Midwife and have been using the epi no now with my clients for the last 12 years and it is very rare that the women tear on a first birth and need stitching.. it is popular in Europe and Australia and Canada and here in Israel and you will not stay stretched out after the birth, so don’t worry about that
**Note for readers – this commenter is a representative of epi-no**
The Epi-no is not supported by good evidence – only small studies sponsored by the company. A well conducted large study has recently been published http://www.ncbi.nlm.nih.gov/pubmed/26924418 that concluded: “Antenatal use of the Epi-No(®) device is unlikely to be clinically beneficial in the prevention of intrapartum levator ani damage, or anal sphincter and perineal trauma.” The current state guidelines here (Queensland, Australia) warn against the use of these devices and there are concerns about long term outcomes (years) for the pelvic floor after such frequent and extensive stretching.
I also rarely see tearing and my approach is to support physiology and instinct: https://midwifethinking.com/2015/09/09/supporting-womens-instinctive-pushing-behaviour-during-birth/ Women don’t need devices. Our job as midwives is to promote and support physiology and reinforce women’s trust in their own bodies. Please see the International Confederation of Midwives’ position statement on the ‘appropriate use of intervention in childbirth’:
http://www.internationalmidwives.org/assets/uploads/documents/Position%20Statements%20-%20English/PS2011_003%20ENG%20Appropriate%20use%20of%20intervention%20in%20childbirth.pdf
Thank you for your reply. I’m glad to have found your website (and others like it) since it offers a different perspective.
I massaged the perineum with wheat germ oil and gently stretched it when showering each day in the last six weeks of pregnancy. I tore a little with my first baby (3 or 4 stitches) but did not tear with each of my subsequent 5 births. All my babies weighed between 8lb 2oz and 10 lb 4oz. I simply used my fingers and no tool.
Dear midwife, thank you so much for your evidence-supported articles. Could you please explain how this happens? “An episiotomy does not prevent a tear from occurring, instead it increases the chance of a third or fourth degree tear (involving the anal sphincter).” Because doctors advocate
for episiotomy exactly for “protecting the anal sphincter.”, so it would be interesting to know what to reply to them.
I am 6.5 months pregnant and completely terrified at the thought of interventions as unnecessary episiotomy or intrusive hands-on while in such a vulnerable condition as in giving birth.
I usually explain this using prop…. so you can try this at home 😉 Take a piece of paper and hold the two corners. Gently pull creating tension across the width of the paper. Now cut a link in that paper – along the top between where you pulled. Now hold the two corners again and pull creating the same tension. The paper will usually tear now because you have created a weakness in the structure. A perineum will also tear along a weakness you create. So with an episiotomy the risk is that stretching and pressure from the baby’s head extends the cut into a deeper tear.
I hope that makes sense 🙂
And many doctors are aware of the evidence and avoid an episiotomy even during a ventous birth because of the risk it extending.
Re. Unnecessary interventions – find out what the normal practice is of your care provider and/or birth setting. This will have a greater influence over your birth experience than your wishes (unfortunately)
Thank you very much. I really can’t see the logic of still doing episiotomies to prevent tears, when they actually cause tears. I mean, it’s not even in the advantage of the doctor. ?? I’ll discuss it with my gynecologist..
I’d have one more question if you may. I read somewhere in your articles about “women not instructed to rest during labour, so they eventually get too tired in the end” (I’m paraphrasing). Could you say more on that topic please, or direct me to an article if it’s already stated? Until now I have only heard of the importance of moving around when labour starts.
There is no logic but there is still a cultural/historical belief that episiotomy can prevent tearing. Practice is really evidence-based it is culture-based. The research = episiotomy increases the risk of a significant tear (3rd / 4th degree) AND does not heal as well as a tear and causes more pain postnatally.
The idea of ‘active’ birth is about encouraging women to get their baby out within prescribed timeframes (for hospitals). Early labour can take a long time. The hormones involved make the woman ‘drowsy’ and dampen the neocortex: https://midwifethinking.com/2017/02/03/understanding-and-assessing-labour-progress/ this helps women to move into established labour. Lots of action and thinking and moving can actually interfere with this. A common problem with first labours is that in early labour women become really active trying to make it happen quicker. This interferes with the hormones and by the time they are in established labour they are utterly exhausted and worn out = epidural and intervention. Early labour is about getting yourself settled into the birth space and trying to relax and rest to allow the oxytocin to build and the adrenaline to drop… that will create the conditions for established labour. Instinctive movements in established labour are common and help the baby move through the pelvis. Conscious / prescribed movements are only helpful with an epidural when instincts and body-brain feedback are prevented. Women know how to birth – they don’t need instructions.
To be honest with you. Where you give birth ie. the culture of the birth setting and the people who care for you will have the biggest influence over your birth outcome. They either understand physiology and how to support it… or don’t.
Recently I received an explanation as to the episiotomy-practices of the hospital where I will give birth: if they see that you are going to tear ( =skin turns white) somewhere sideways, they let the tear happen. But if they see that you are going to tear vertically, then they do an episiotomy sideways to ‘divert’ a tear that could damage the anal sphincter. What is your opinion on that practice? Does it indeed work as intended?
The research is clear that episiotomy increases your chance of an extended tear. So whilst the practice you describe has a theory behind it… it is not supported by evidence. And it is confusing because you don’t see where the internal vaginal wall is tearing – it happens inside out of view. They are basing this on what the external skill is doing. Strange.
They must be used to births with the woman on her back exposing her perineum in a well lit environment – all of which works against physiology and increases the chance of tearing.
Forward leaning positions take the pressure off the perineal area near the anal sphincter.
The best approach to avoiding tears is to promote women’s instinctive behaviours during birth. https://midwifethinking.com/2015/09/09/supporting-womens-instinctive-pushing-behaviour-during-birth/
I’d be finding out what the episiotomy rate is in the hospital you are giving birth in… and their rate of physiological birth. What you are being told raises concerns.
You can write in your birth plan that you do not give consent for an episiotomy even if there are concerns about tearing. Legally they cannot do one without your consent.
I’m reading these comments and article with great interest, as I have always followed the above methods for reducing tears. But now a RCOG care bundle as commenced at my hospital. Basically saying that episiotomies and hands on technique have now been found to reduce third degree tears. All midwives/doctors are being encouraged (after discussion with the woman) to use hands on to deliver baby and shoulders, no traction to deliver shoulders, and consider episiotomy if the perineum is rigid/ button holing etc. They expect the third degree rate to decrease by half in the 4 hospitals that have commenced the care bundle. I have never done a episiotomy unless there has been fetal distress, so will have to completely change the way I practice. just wondered if you have any thoughts on this?
This is a great example of how culture influences the interpretation and implementation of evidence. The incidence of 3rd degree tearing is low – usually around the 1% mark in hospitals. It is particularly associated with syntocinon for multips, forceps delivery and extended episiotomies, yet these practices are not stopped. Instead lots of women are subjected to unnecessary interference and genital mutilation because it may lower a small % to a smaller %. I would be very interested to see the rates of intact, 1st and 2nd degree tears in the ‘care bundle’ hospitals (likely they will be significantly lower and the episiotomy rates higher). There will also likely be increased PPH due to the physical and psychological effect of interference and cutting the body at this point in labour.
Most importantly are women being given adequate information about this and giving consent for these interventions? I have heard this is often not the case.
It is time we focussed on promoting and supporting physiology as a risk management strategy – not routine intervention and disempowerment. Midwives need to say enough is enough and refuse to implement this ‘care bundle’ as it contradicts their professional standards and philosophy. We need to take responsibility for our own practice and stop colluding in disrespectful maternity care. Midwives are in a powerful position – we provide the face-to-face care of women – we need to use that power to advocate for women.
I agree with your comments, so often women aren’t given the true figures for how successful an intervention will be at preventing adverse outcomes. I will really struggle to perform an episiotomy when I have never practised this way. But there is a lot of pressure now to do them. I have seen rigid perineums that do eventually stretch and remain intact, but under these guidelines an episiotomy would be recommended. I guess it’s all about the cost of providing after care for women with anal sphincter tear. The rate at our hospital is currently 6%.
6% is huge. There needs to be an audit of practice to see how this is happening. Directed pushing? Birth position? Is there access to waterbirth? Are these tears happening during an instrument birth? Is this the rate when women are cared as per the blog post?
I have attended hundreds of births practising in the way described in this post. I have only seen one 3rd degree tear in that time (standing up birth) following a physiological undisturbed birth. Lots of ‘rigid’ perineums that ‘give’ without tearing or with minor tearing. Why are you going to change the way you practise if you know it works? You are an autonomous practitioner – professionally obliged to centre care around the woman and evidence. Not around hospital preferences. You need to tell the women you care for about this ‘bundle’ (risks and benefits) and ensure they consent to any intervention. Just because something is recommended doesn’t mean you have to do it or that the woman has to comply.
Okay, that’s very interesting to know that you don’t see on the external skin where/if an internal tear will happen. Best way to avoid a nasty tear at a nasty place is good positioning and instinctive pushing…check! That’s enough to know for me in order to ask for no episiotomy.
(But still, just out of curiosity, if you *do* see externally that there’s a tear on the way, aren’t there increased chances that it will go deeper too?)
Thank you for all the suggestions! Indeed, if the woman herself doesn’t request to birth in a different position, most doctors prefer you on your back. Unfortunately there’s a policy here (Belgium) that the obstetrician *has* to attend the last minutes of labour and the birth of the baby, even if you have an independent midwife with you. But despite that I’m in bliss now… I just changed OBs! I left one who doesn’t do waterbirth and apparently does standard episiotomies just to get it over with quickly (!!!), to one who doesn’t do standard cuts..and who respects your wish to birth in water or other positions. I’m so relieved… And I also just started going to a midwife for appointments instead of the gynecologist (will only go a couple of times now to get to know him better..). It feels so much more “normal”! She doesn’t do sonograms, but does palpations of course, and it was the first time I experienced that. Such a difference to having a sonogram! Funnily enough, I felt now more connected to the baby without seeing it than when I would see it on the screen (which was also nice of course). Midwives are wonderful. Even though she has been more medically schooled than I’d ideally want, she is someone who loves midwifery, listens and respects, and I feel safe with her. She’ll come at home when I’m in labour to support me and stay as long as possible at home..and then will come to the hospital too. I’m so happy with this solution! I know that still a lot can go wrong when in labour… But before meeting the midwife and changing doctors I felt like a trapped animal who will have to fight, and I already knew that my labour would stall like that. It was so terrible. Thank God, I feel liberated now. And your blog has helped me tremendously.
Congratulations. Your care provider has a powerful influence on your birth experience and you have now chosen one that is aligned with your approach to birth 🙂
And – no, I would cut a woman to prevent a tear. A tear is less painful and heals better than a neat cut through muscle.
Waterbirth reduces the chance of tearing – it also reduces care providers access you for perineum 😉
Good luck with your birth – it would be lovely if you come back and let us know how it goes.
Thank you! It’s still quite some weeks to go, but I’ll surely come back then. 🙂
Hi Rachel!! I absolutely love all your articles, and thoroughly enjoy reading them!
I am currently writing an article on episiotomies and came across some research that I’m not sure what to make of.
https://www.ncbi.nlm.nih.gov/pubmed/25203655
The study is called “The association of episiotomy with obstetric anal sphincter injury–a population-based matched cohort study.”
According to the study, episiotomies in fact do protect women’s perineums, and the reason for more cases of OASIS in women with episiotomies was because the same risks of OASIS were noticed by the care providers so they had a chance to react.
I know this conclusion doesn’t sit right with me, but I can’t find a way around it. The study was, after all, done with a large population.
Could you please help me figure this out?
Thanks!
Medio-lateral episiotomy can reduce the chance of a 3/4 degree tear. However it does not protect the perineum. 100% of women with an episiotomy have perineal damage (a cut) with potentially long term harm (damage to clitoral tissue).
I’ve written more about episitomy in this post: https://midwifethinking.com/2018/05/09/the-perineal-bundle-and-midwifery/
There are other factors that reduce the chance of perineal tearing more (see article). Yet, they are not advocated by clinicians. Also bear in mind that this study was undertaken with a population of women birthing in hospital with interventions and likely semi-supine… all factors that increase the chance of 3/4 degree tearing.
We cannot apply these findings to undisturbed physiological birth.
Women need to be given information to make their own decision about episiotomy… do they want 100% chance of a perineal cut or a 3% chance of a significant tear? What methods/approaches do they want to use to reduce tearing eg. not being directed when pushing, instinctive birth positions etc.
Okay, that makes much better sense. Thank you!
What if, at your first birth you had a 3rd degree tear. Is there anything additional you can do to protect/ prepare the perineum during the next pregnancy and/or birth? Has there been any research regarding the chances of further or worse tears for subsequent births?
A woman who experiences a significant tear with her first birth is “no more likely to have an operative birth or another severe perineal tear in a subsequent birth.” https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/1471-2393-13-89
Physiological, instinctive birth protects the perineum. So all of the information in the post (and my book) is applicable to a woman with a previous tear.
I did use an aniball (epino) in preparation for my 2th birth. My first was a preterm birth af 20 weeks, so not comparable because my little boy was only 315 grams. Practicing with the aniball gave me confidence, it helped me to feel familiar with the stretchy feeling and I was able to practice pushing and to see that I was able to do it. I practiced relaxation. I have a history of sexual abuse and vaginismus, so releasing the tension surrounding birth and gaining confidence was crucial for me. Eventually I gave birth within an hour after waking up from contractions, unplanned and unassisted at home with only a small amount of water in my bathtub. My midwife and friend were to late to attend the birth, let alone go to the hospital. When the head descended I recognized the feeling and that helped me not to panic. I never actively pushed, my daughter just flew out of the birth canal. And… I had an intact perineum. I never believed the epino would decrease the change of perineal tearing, but it absolutely did help me to have more confidence and a calmer birth.